Prostate Cancer Screening Controversies: Making Sense of Changing Guidelines
I still remember the confusion on my friend David’s face when his doctor told him the PSA test he’d been getting annually for years was “no longer recommended.” Like many men, he’d been diligently following his doctor’s advice, only to suddenly hear that the medical community had changed its mind. “So was I wasting my time all these years?” he asked me. “Or am I putting myself at risk by stopping now?”
This confusion isn’t unique to David. For decades, prostate cancer screening has been one of medicine’s most contentious topics, with guidelines changing repeatedly and different medical organizations offering conflicting advice. As someone who’s spent years advocating for men’s health, I’ve witnessed firsthand how these shifting recommendations leave both patients and physicians bewildered.
The controversy centers on a fundamental question: Does routine PSA screening save enough lives to justify the potential harms of overdiagnosis and overtreatment? Let’s unpack this complex issue and help you make sense of the changing landscape.
The Evolution of Prostate Cancer Screening Guidelines
To understand today’s controversy, we need to look at how prostate cancer screening recommendations have evolved over time.
The Early Days: Widespread Screening (1990s-2000s)
When PSA testing became widely available in the early 1990s, it was quickly embraced as a simple blood test that could potentially detect prostate cancer early. During this period:
- Most medical organizations recommended annual PSA testing for men starting at age 50
- Some advocated starting at age 40 for high-risk groups
- Digital rectal exams (DREs) were routinely performed alongside PSA tests
- Little attention was paid to potential harms of screening
The result was a dramatic increase in prostate cancer diagnoses. Between 1986 and 1992, the incidence of prostate cancer in the United States increased 82%, largely attributed to PSA testing.
The Backlash: Questioning the Value (2008-2012)
As more data accumulated, concerns about overdiagnosis and overtreatment grew. The turning point came in 2012 when the U.S. Preventive Services Task Force (USPSTF) issued a controversial Grade D recommendation against PSA-based screening for all men, regardless of age or risk factors.
Their rationale included:
- Limited evidence that screening reduced overall mortality
- Significant harms from false positives and unnecessary treatments
- Concerns that many detected cancers would never become clinically significant
This recommendation sent shockwaves through the medical community and created widespread confusion among patients.
The Current Era: Shared Decision-Making (2018-Present)
In 2018, the USPSTF revised its stance, upgrading its recommendation to a Grade C for men aged 55-69, emphasizing individualized decision-making. Most major medical organizations now advocate for a more nuanced approach that considers:
- Individual risk factors
- Patient preferences and values
- Shared decision-making between patient and provider
- Selective use of screening in appropriate populations
Understanding the Major Studies That Shaped the Debate
The controversy around prostate cancer screening stems largely from seemingly contradictory results from major clinical trials. Let’s examine the two most influential studies:
The European Randomized Study of Screening for Prostate Cancer (ERSPC)
This large European trial involving over 162,000 men found that PSA screening reduced prostate cancer mortality by approximately 21% after 16 years of follow-up. More recent data from 2025 shows:
- Men who consistently avoided screening had a 45% higher risk of dying from prostate cancer
- Those who attended screening appointments had a 23% lower risk of dying from prostate cancer
- The number needed to invite (NNI) to prevent one prostate cancer death decreased from 742 to 570 over time
- The number needed to diagnose (NND) to prevent one death decreased from 26 to 18
These findings suggest a clear mortality benefit from screening, particularly with longer follow-up.
The Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial
This American study of nearly 77,000 men found no mortality benefit from PSA screening. However, subsequent analyses revealed significant contamination in the control group—up to 90% of men in the “non-screening” arm actually received PSA testing outside the study.
Dr. Ruth Etzioni, a biostatistician at Fred Hutchinson Cancer Center, explains: “When we account for the high rate of screening in the control arm, the PLCO results are actually consistent with the European trial. Both suggest a benefit to organized screening compared to no screening.”
The Harms of Screening: Understanding Overdiagnosis and Overtreatment
The potential benefits of prostate cancer screening must be weighed against its harms. The two most significant concerns are overdiagnosis and overtreatment.
Overdiagnosis: Finding Cancers That Would Never Cause Harm
Autopsy studies reveal that many men die with prostate cancer, not from it. Research shows:
- 68-77% of men aged 60-79 have microscopic prostate cancer at autopsy
- Many of these cancers would never have caused symptoms during the man’s lifetime
- Estimates suggest 23-66% of screen-detected prostate cancers represent overdiagnosis
Dr. Michael Barry, a professor of medicine at Harvard Medical School, notes: “The problem isn’t finding prostate cancer—it’s distinguishing the tigers from the pussycats. Many prostate cancers grow so slowly that they would never threaten a man’s life, yet once diagnosed, they cause significant anxiety and often lead to treatment.”
Overtreatment: The Cascade of Interventions
Until recently, most men diagnosed with prostate cancer received aggressive treatment, regardless of the cancer’s risk level. This led to:
- Unnecessary surgeries and radiation treatments
- Significant side effects including incontinence and erectile dysfunction
- Reduced quality of life without clear survival benefit for many men
A study published in the Journal of the American Medical Association found that 91% of men in the PLCO trial received aggressive treatment for their prostate cancer, even though many had low-risk disease that could have been safely monitored.
The Psychological Impact of Prostate Cancer Diagnosis
Beyond the physical harms of unnecessary treatment, the psychological impact of a cancer diagnosis is substantial:
- Increased anxiety and depression following diagnosis
- Higher rates of cardiovascular events in the year following diagnosis
- Elevated suicide risk, particularly in the first year after diagnosis
These psychological harms affect not only the patient but also their family members and loved ones.
Current Guidelines: Who Should Be Screened and When?
With all this conflicting information, what do today’s guidelines actually recommend? While there are still differences between organizations, there’s growing consensus around several key points:
American Urological Association (AUA) Recommendations
- Ages under 40: Routine screening not recommended
- Ages 40-54: Selective screening for high-risk men (African American, family history)
- Ages 55-69: Shared decision-making approach; screening every 2-4 years if chosen
- Ages 70+: Screening not recommended for men with less than 10-15 year life expectancy
American Cancer Society (ACS) Recommendations
- Age 50: Discussion about screening for average-risk men with at least 10-year life expectancy
- Age 45: Discussion about screening for high-risk men (African American, family history of prostate cancer diagnosed before age 65)
- Age 40: Discussion about screening for men at even higher risk (multiple family members diagnosed at early age)
- Follow-up: If PSA <2.5 ng/mL, screening every 2 years; if PSA ≥2.5 ng/mL, annual screening
U.S. Preventive Services Task Force (USPSTF) Recommendations
- Ages 55-69: Individual decision based on values and preferences (Grade C recommendation)
- Ages 70+: Recommends against PSA-based screening (Grade D recommendation)
Dr. James Eastham, Chief of Urology at Memorial Sloan Kettering Cancer Center, observes: “The 2025 guidelines reflect a more nuanced understanding of prostate cancer risk. We’re moving away from one-size-fits-all recommendations toward personalized screening strategies based on individual risk factors.”
Special Considerations for High-Risk Populations
The benefit-to-harm ratio of prostate cancer screening varies significantly across different populations. Two groups deserve special attention:
African American Men
Black men face a substantially higher risk of developing and dying from prostate cancer:
- 1 in 6 Black men will be diagnosed with prostate cancer in their lifetime
- Black men are more than twice as likely to die from prostate cancer compared to white men
- The disease often appears earlier and in more aggressive forms
For these reasons, most guidelines recommend earlier screening for African American men, typically starting at age 45 or even 40.
Men with Family History
Family history significantly increases prostate cancer risk:
- Men with a first-degree relative with prostate cancer have twice the risk
- Risk increases further with multiple affected relatives
- Earlier age of diagnosis in relatives suggests higher genetic risk
The National Comprehensive Cancer Network (NCCN) recommends that men with a family history begin screening discussions at age 45, or 10 years before the earliest diagnosis in the family.
Innovations Improving the Screening Paradigm
The good news is that advances in technology and approach are helping to address many of the historical concerns about prostate cancer screening.
Risk-Stratified Screening
Rather than applying the same screening protocol to all men, risk-stratified approaches tailor screening based on individual risk factors:
- Baseline PSA levels at a younger age (40-45) to establish risk
- Family history and genetic risk assessment
- Race and ethnicity considerations
- Consideration of overall health status and comorbidities
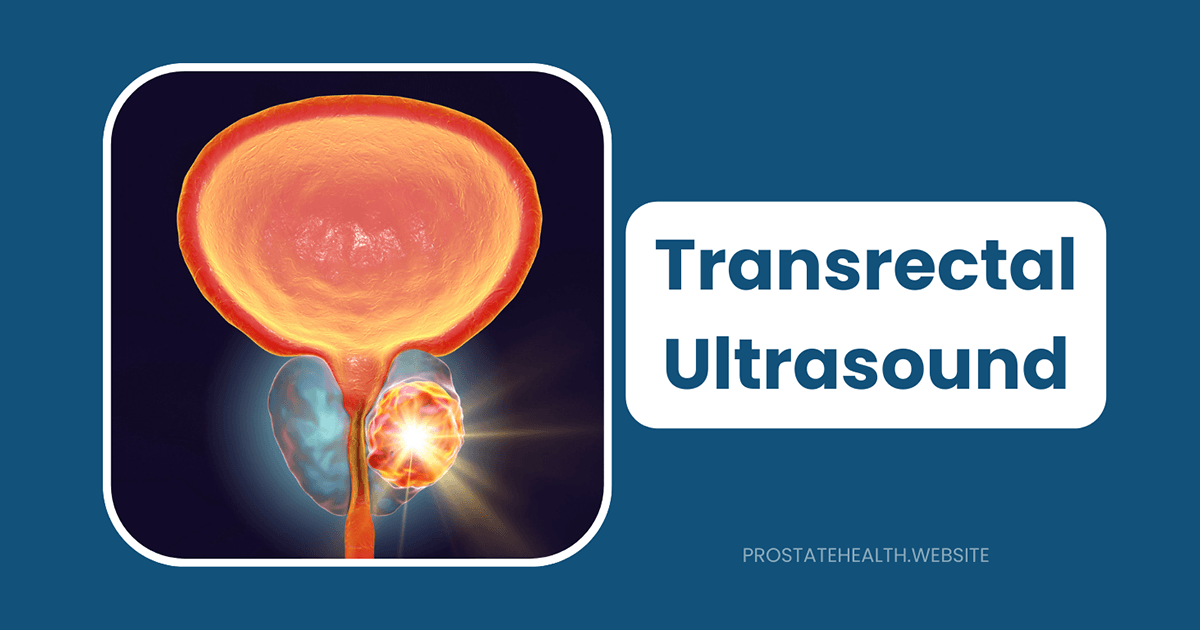
Advanced Imaging
Multiparametric MRI (mp-MRI) has revolutionized prostate cancer detection:
- Can visualize suspicious areas before biopsy
- Reduces unnecessary biopsies by 28-33%
- Improves detection of clinically significant cancers
- Decreases detection of insignificant cancers
Biomarker Tests
New blood and urine tests improve upon PSA’s limitations:
- 4Kscore: Combines four prostate-specific kallikreins with clinical information
- Prostate Health Index (PHI): Combines total, free, and [-2]proPSA
- SelectMDx: Urine-based test measuring mRNA biomarkers
- Stockholm3: Combines protein markers, genetic markers, and clinical variables
A 2025 study found that using PSA screening followed by the Stockholm3 test and MRI could reduce overdiagnosis by 60% while maintaining mortality benefits.
Active Surveillance
Perhaps the most significant advance is the widespread adoption of active surveillance for low-risk prostate cancer:
- Regular monitoring instead of immediate treatment
- Intervention only if cancer shows signs of progression
- Preserves quality of life while maintaining cancer control
- Now recommended as the preferred approach for low-risk disease
Dr. Laurence Klotz, a pioneer of active surveillance, notes: “The adoption of active surveillance has been the single most important advance in addressing overtreatment. We now recognize that many prostate cancers can be safely monitored, sparing men unnecessary treatments and their side effects.”
Making Your Personal Decision About Screening
With all this information, how should you approach the decision about prostate cancer screening? Here’s a framework to guide your thinking:
1. Understand Your Personal Risk Factors
- Age: Your risk increases significantly after age 50
- Race: African American men have higher risk
- Family history: First-degree relatives with prostate cancer increase your risk
- Genetic factors: Certain genetic mutations (BRCA1/2, Lynch syndrome) increase risk
2. Consider Your Values and Preferences
- How do you feel about the possibility of finding a cancer that might never cause harm?
- How concerned are you about missing a potentially lethal cancer?
- How would you weigh quality of life versus longevity if faced with treatment decisions?
- What is your tolerance for medical uncertainty?
3. Have a Detailed Conversation with Your Healthcare Provider
Discuss:
- Your specific risk factors
- The potential benefits and harms of screening in your case
- What a positive test would mean and what next steps would involve
- Alternative or supplemental testing options beyond standard PSA
4. Make an Informed Choice
Remember that there is no universally “right” decision about prostate cancer screening. The best choice is one that aligns with your values, risk factors, and preferences after considering all available information.
The Future of Prostate Cancer Screening
Looking ahead, several developments promise to further improve the benefit-to-harm ratio of prostate cancer screening:
Genetic Risk Assessment
Emerging research suggests that genetic testing could help identify men at highest risk for aggressive prostate cancer:
- Germline testing for BRCA1/2 and other mutations
- Polygenic risk scores combining multiple genetic variants
- Integration of genetic risk with clinical risk factors
Artificial Intelligence
AI algorithms are being developed to:
- Better interpret prostate MRI images
- Predict which prostate cancers are likely to progress
- Integrate multiple data points to personalize screening recommendations
Liquid Biopsies
Blood tests that detect circulating tumor DNA and other cancer markers may eventually:
- Provide non-invasive cancer detection
- Distinguish aggressive from indolent cancers
- Monitor treatment response and recurrence risk
Dr. Peter Carroll, a urologist at UCSF, predicts: “Within the next decade, I believe we’ll move beyond the PSA-only paradigm to a more sophisticated, multimodal approach that better distinguishes lethal from non-lethal prostate cancer. This will finally resolve many of the controversies that have plagued prostate cancer screening.”
Conclusion: Finding Clarity Amid Controversy
The prostate cancer screening debate reflects the challenge of balancing population health with individual care. While no screening test is perfect, the evolving approach to prostate cancer detection represents a more thoughtful balance of benefits and harms.
For men facing this decision today, the key takeaways are:
- One size doesn’t fit all – Screening decisions should be individualized based on risk factors and personal preferences
- Shared decision-making is essential – Work with your healthcare provider to understand the implications of screening in your specific case
- The landscape continues to improve – Advances in technology and approach are addressing many historical concerns about screening
- High-risk men benefit most – African American men and those with family history should consider earlier and potentially more frequent screening
- If cancer is found, treatment isn’t always necessary – Active surveillance provides a safe option for many men with low-risk disease
By understanding the nuances of this complex issue, you can make an informed decision that’s right for you—navigating the controversy rather than being paralyzed by it.
References:
- American Urological Association
- American Cancer Society
- U.S. Preventive Services Task Force
- European Association of Urology
- ZERO – The End of Prostate Cancer