PSA Testing: When Should You Start and How Often?
I remember sitting in my doctor’s office at 45, completely caught off guard when he asked if I wanted to start PSA testing. Like many men, I had heard of prostate cancer but knew little about screening timelines or what a PSA test actually involved. That moment sparked my journey into understanding prostate health—knowledge I wish I’d had years earlier.
PSA (Prostate-Specific Antigen) testing remains one of our most valuable tools for early detection of prostate cancer, yet confusion abounds about when to start and how frequently to test. This isn’t just a medical decision—it’s a deeply personal one that requires understanding your own risk factors and comfort level with screening.
What Exactly Is a PSA Test?
Before diving into timing recommendations, let’s clarify what we’re talking about. A PSA test is a simple blood test that measures the amount of prostate-specific antigen in your bloodstream. PSA is a protein produced by both cancerous and non-cancerous tissue in the prostate.
While elevated PSA levels can indicate prostate cancer, they can also result from other conditions like benign prostatic hyperplasia (BPH), prostatitis, or even recent ejaculation. This is why PSA testing is just one piece of the diagnostic puzzle.
Age-Based PSA Testing Guidelines: When Should You Start?
The question of when to begin PSA testing has evolved over the years as research has refined our understanding of prostate cancer risks and screening benefits. Current guidelines from major medical organizations provide a framework, but remember—these are starting points for discussion with your healthcare provider.
For Men Under 40
According to the American Urological Association (AUA), routine PSA screening is not recommended for men under 40. The prevalence of prostate cancer in this age group is extremely low, and the potential harms of screening (anxiety, unnecessary procedures) typically outweigh the benefits.
Exception: If you have a strong family history of early-onset prostate cancer (multiple first-degree relatives diagnosed before 65), your doctor might recommend baseline testing earlier.
For Men Ages 40-54
For most men in this age range, routine screening isn’t recommended unless you have risk factors that place you in a higher-risk category. These risk factors include:
- African American heritage – Black men have approximately double the risk of developing and dying from prostate cancer compared to other ethnic groups
- Family history – Having a father or brother diagnosed with prostate cancer, especially before age 65
- Known genetic mutations – Particularly BRCA1/2 or Lynch syndrome
If you fall into any of these higher-risk categories, the conversation about PSA testing should begin around age 40-45. Your doctor might recommend establishing a baseline PSA level and then determining follow-up screening frequency based on that result.
For Men Ages 55-69
This is the age range where the evidence for PSA screening benefits is strongest. The AUA and many other organizations recommend that men in this age group engage in shared decision-making with their healthcare providers about PSA screening.
Research shows that regular screening in this age group can reduce prostate cancer mortality. According to Johns Hopkins Medicine, men aged 55 to 69 benefit most from screening as they are most likely to develop prostate cancer during this period.
For Men Age 70 and Older
For men 70 and older, routine PSA screening is generally not recommended, particularly for those with a life expectancy under 10-15 years. However, men in excellent health with a longer life expectancy may still benefit from selective screening after discussing with their doctor.
How Often Should You Get Tested?
Once you’ve decided to begin PSA testing, the next question is frequency. The days of automatic annual PSA tests are largely behind us, with research suggesting that less frequent testing may provide similar benefits with fewer downsides.
Risk-Based Testing Intervals
Current recommendations suggest tailoring the frequency of PSA testing based on your baseline PSA level and risk factors:
For Average-Risk Men:
- If your PSA is less than 1 ng/mL: Testing every 2-4 years is generally sufficient
- If your PSA is between 1-3 ng/mL: Testing every 1-2 years is typically recommended
- If your PSA is above 3 ng/mL: Your doctor will likely recommend additional testing or more frequent monitoring
For High-Risk Men:
- If your PSA is 3 ng/mL or less: Testing every 1-2 years
- If your PSA is above 3 ng/mL: Your doctor will likely recommend additional evaluation
Dr. William Catalona, a pioneering researcher in prostate cancer screening, notes: “The higher your baseline PSA level, the more frequently you should be screened. Men with very low PSA levels may need less frequent testing, while those with borderline or rising levels need closer monitoring.”
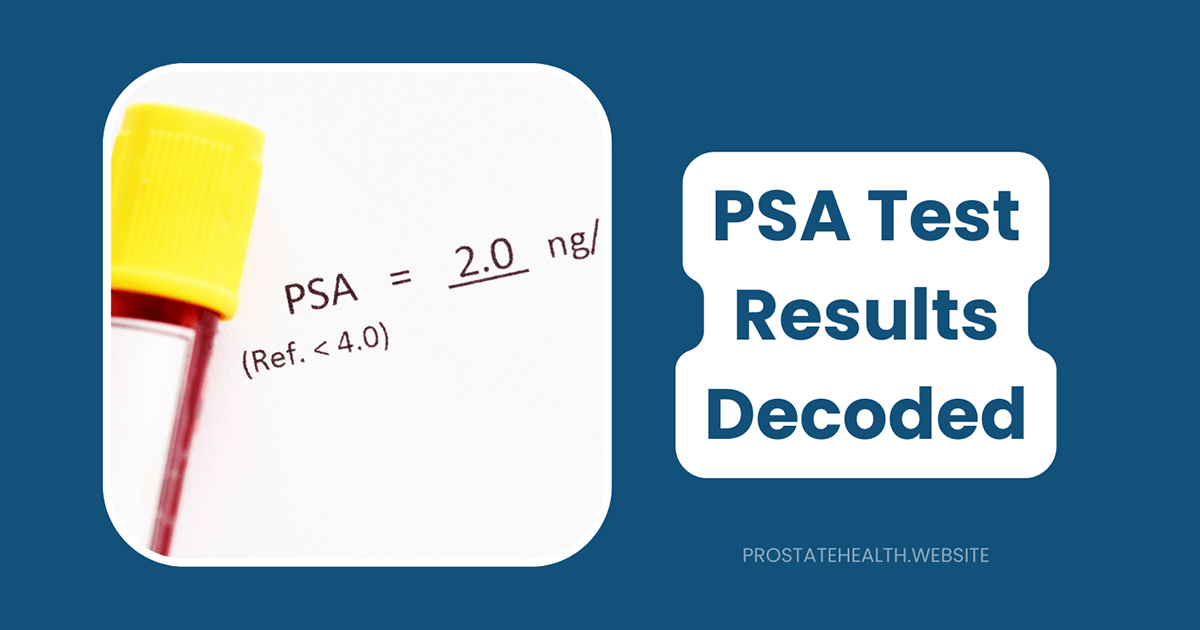
Understanding PSA Levels by Age
What constitutes a “normal” PSA level changes as you age. The prostate naturally grows larger over time, which can lead to higher PSA levels even in the absence of cancer.
Age-specific PSA reference ranges commonly cited include:
- 40-49 years: PSA below 2.5 ng/mL
- 50-59 years: PSA below 3.5 ng/mL
- 60-69 years: PSA below 4.5 ng/mL
- 70+ years: PSA below 6.5 ng/mL
However, it’s important to note that these are general guidelines. What matters most is not a single PSA reading but rather:
- How your PSA changes over time (PSA velocity)
- Your PSA density (PSA level relative to prostate size)
- The ratio of free PSA to total PSA
These nuanced measurements provide more context than a single number and help reduce unnecessary biopsies.
Beyond the Numbers: What Happens After an Elevated PSA?
An elevated PSA doesn’t automatically mean you have cancer. In fact, about 75% of men with PSA levels between 4 and 10 ng/mL do not have prostate cancer. Before jumping to conclusions or invasive procedures, your doctor may:
- Repeat the PSA test – PSA levels can fluctuate due to many factors
- Perform additional blood tests – Such as the 4Kscore or PHI (Prostate Health Index)
- Recommend an MRI – To visualize the prostate before deciding on a biopsy
- Consider a digital rectal exam (DRE) – To physically check for prostate abnormalities
If these follow-up measures still suggest a potential problem, a prostate biopsy might be recommended. Modern approaches often use MRI guidance to target suspicious areas rather than the traditional random sampling method.
Special Considerations for High-Risk Groups
African American Men
Black men face a substantially higher risk of developing prostate cancer and tend to develop more aggressive forms of the disease at younger ages. The American Cancer Society recommends that African American men begin the screening discussion at age 45 rather than 50.
Some experts even suggest baseline testing at age 40 for Black men to establish their personal PSA trajectory. Regular screening is particularly important for this high-risk group.
Men with Family History
If you have a father, brother, or multiple male relatives who have had prostate cancer, your risk is significantly elevated. The more relatives affected and the younger they were at diagnosis, the higher your risk.
For men with a strong family history, consider:
- Starting screening 5-10 years before the age your youngest affected relative was diagnosed
- More frequent testing intervals (annually rather than every 2-4 years)
- Additional genetic testing to assess hereditary cancer risk
Making Your Decision: The Shared Decision-Making Approach
The decision to undergo PSA testing isn’t one-size-fits-all. The U.S. Preventive Services Task Force emphasizes a shared decision-making approach where you and your doctor weigh several factors:
- Your personal risk level
- Your values regarding early detection
- Your concerns about false positives or overdiagnosis
- Your preferences regarding potential treatment if cancer is found
This conversation should include a frank discussion of both the potential benefits (early cancer detection, peace of mind) and potential harms (anxiety, unnecessary procedures) of PSA testing.
The Future of Prostate Cancer Screening
PSA testing continues to evolve, with newer approaches aiming to increase accuracy and reduce unnecessary biopsies. Some promising developments include:
- Multi-parametric MRI before biopsy to better visualize suspicious areas
- Genetic risk scores to personalize screening recommendations
- Biomarker panels that combine PSA with other markers for better specificity
- STHLM-3 test which combines clinical variables and blood biomarkers for improved accuracy
These advances may soon allow for more personalized screening approaches based on individual risk profiles rather than age alone.
Taking Action: Next Steps for Prostate Health
Whether you decide to begin PSA testing now or later, there are steps every man can take to support prostate health:
- Know your family history – Talk to relatives about prostate cancer in your family
- Maintain a healthy lifestyle – Evidence suggests that diet, exercise, and maintaining a healthy weight may reduce prostate cancer risk
- Be aware of symptoms – While early prostate cancer rarely causes symptoms, be alert for urinary changes, erectile dysfunction, or bone pain
- Have the conversation – Discuss PSA testing with your healthcare provider at your next check-up
The Bottom Line
PSA testing remains an important tool for early detection of prostate cancer, but the decision of when to start and how often to test should be individualized. By understanding the guidelines, knowing your personal risk factors, and having informed conversations with your healthcare provider, you can make the choice that’s right for you.
Remember, the goal isn’t just early detection—it’s maintaining quality of life while reducing your risk of dying from prostate cancer. The right screening approach helps achieve that balance.
Have you had conversations with your doctor about PSA testing? What factors influenced your decision? Share your experience in the comments below to help other men navigate this important health decision.